[Product Promotion] LAG-3 Target Cell Screening Model
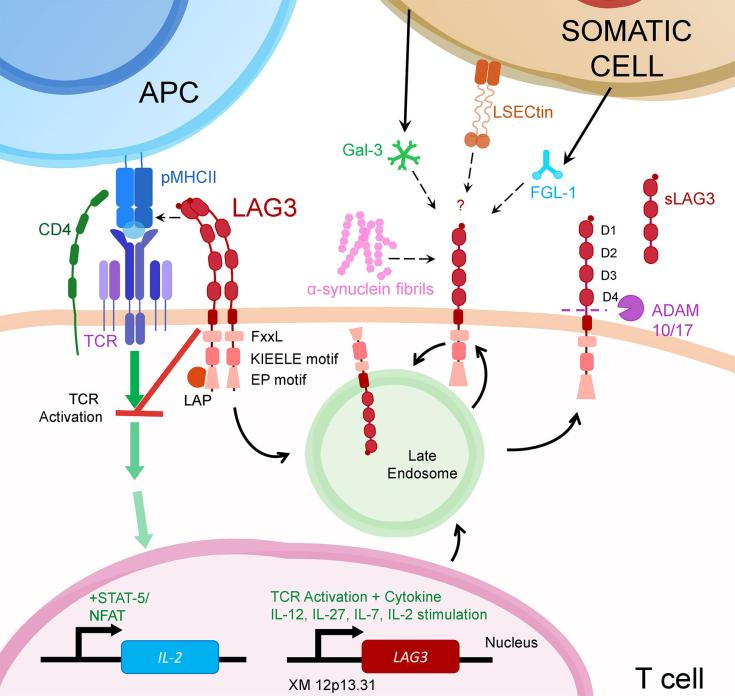
Lymphocyte-activation gene 3 (LAG-3), also known as CD233, was discovered by Triebel et al. in 1990. LAG-3 is a type I transmembrane protein that belongs to the immunoglobulin (Ig) superfamily and is mainly expressed on the surface of T cells and NK cells. The LAG-3 gene is located on chromosome 12. The LAG-3 protein is composed of three parts: extracellular region, transmembrane region and cytoplasmic region. The extracellular region of LAG-3 has 4 immunoglobulin superfamily similar (IgSF- like) domain (D1-D4). There is a loop structure in the D1 domain, which allows LAG-3 to bind to MHC II (major histocompatibility complex II, MHC II) molecules. The cytoplasmic region of LAG-3 consists of three It consists of three parts: serine phosphorylation site, KIEELE element and glutamate pro-line dipeptide repeat sequence (EP repeat). The KIEELE element is involved in the downstream signal transduction of LAG-3, and it is LAG-3 that regulates T cell function. Necessary. The main ligand of LAG-3 is histocompatibility complex II (major histocompatibility complex II, MHC II), in addition to galectin-3 (Galectin-3), sinusoidal endothelial cell lectin (LSECtin ), FGL1 (fibrinogen-like protein1) and other interactions to regulate T cell responses.
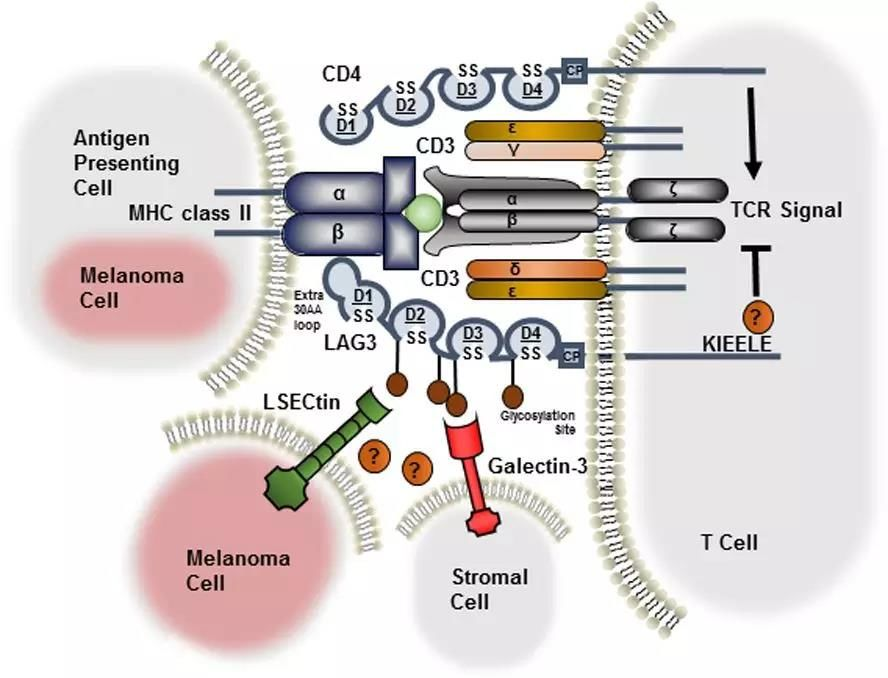
LAG-3 is an inhibitory immune checkpoint of T cells, similar to PD-1 and CTLA-4. When LAG-3 binds to a ligand, it can negatively affect the activity of TCR and regulate the proliferation, activation, function, and function of T cells. Homeostasis, including negative regulation of the proliferation and function of CD4% 2BT cells and CD8% 2BT cells, participates in the inhibitory effect of regulatory T cells (Treg). When in a tumor environment or chronic infection, long-term antigen stimulation will cause the continuous high expression of LAG-3 in T cells, causing T cell exhaustion. Blocking the LAG-3 signaling pathway can promote the recovery of exhausted T cells, regulate the signaling pathways of T lymphocytes and antigen presenting cells (APCs), and play an important role in the adaptive immune response, allowing T cells to regain cytotoxic activity. Reduce the function of regulating T cells to suppress immune response, thereby enhancing the killing effect on tumors. Therefore, LAG-3 has become a very promising target for tumor immunotherapy.
Current status of LAG3-3 target drug development
LAG-3 targeted drugs are currently in clinical trials, and no drugs are on the market. There are mainly two types of LAG-3 modulators used to treat cancer and autoimmune diseases:
(1) Soluble LAG-3 recombinant protein (such as IMP321), has entered the clinical stage, as an antigen-presenting cell activator to enhance the immune response, and can also be used in combination with chemotherapeutic drugs or immunosuppressive drugs to enhance the patient's immune response.
(2) LAG-3 monoclonal antibody drugs, there are currently nearly 30 drugs in clinical trials worldwide, but no drugs are on the market. Among them, the fastest progress is BMS's Relatlimab, which has completed phase II/III clinical research trials and has reached no progress. The primary endpoint of survival (PFS), the trial evaluated the efficacy and safety of Relatlimab in combination with Opdivo (nivolumab) in the treatment of previously untreated patients with metastatic or unresectable melanoma. LAG-3 monoclonal antibody is currently mainly used in combination with other immune checkpoint inhibitors (such as PD-1 monoclonal antibody). There are 13 of the existing 20 NIH clinical trials on LAG-3 that are used in combination with PD-1 inhibitors.
LAG-3 target drug cell screening model
In response to the needs of LAG-3 target drug development and target research, we have developed the LAG-3 series of drug sieve cell lines.
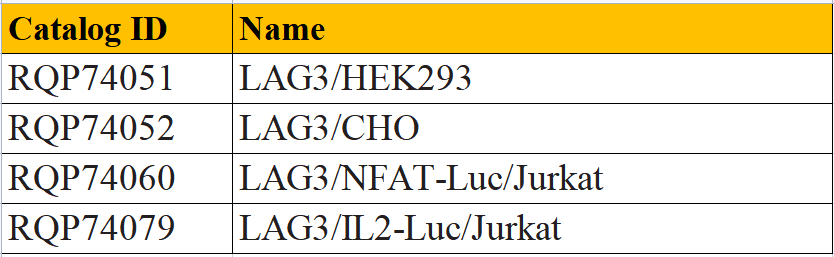
LAG3/HEK293 CBP74051
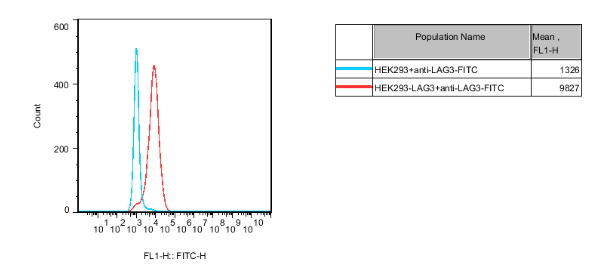
Figure 3. Recombinant HEK293 stably expressing human LAG3.
LAG3/CHO CBP74052
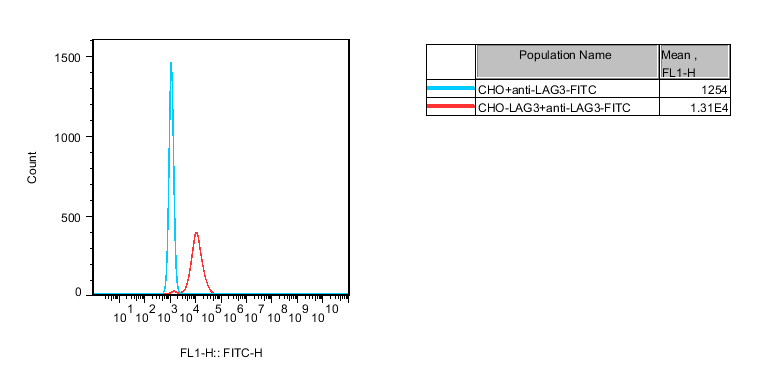
Figure 4. Recombinant CHO cells constitutively expressing human LAG3.
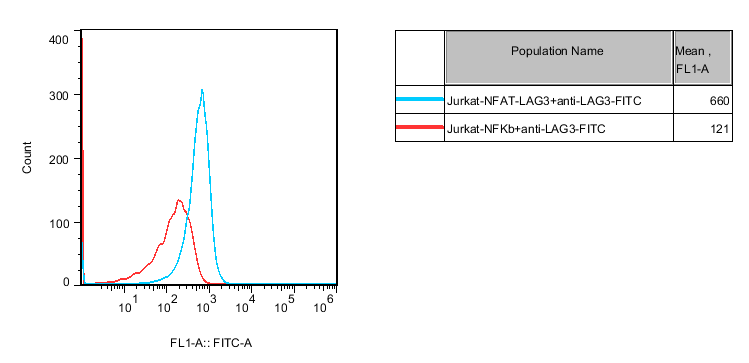
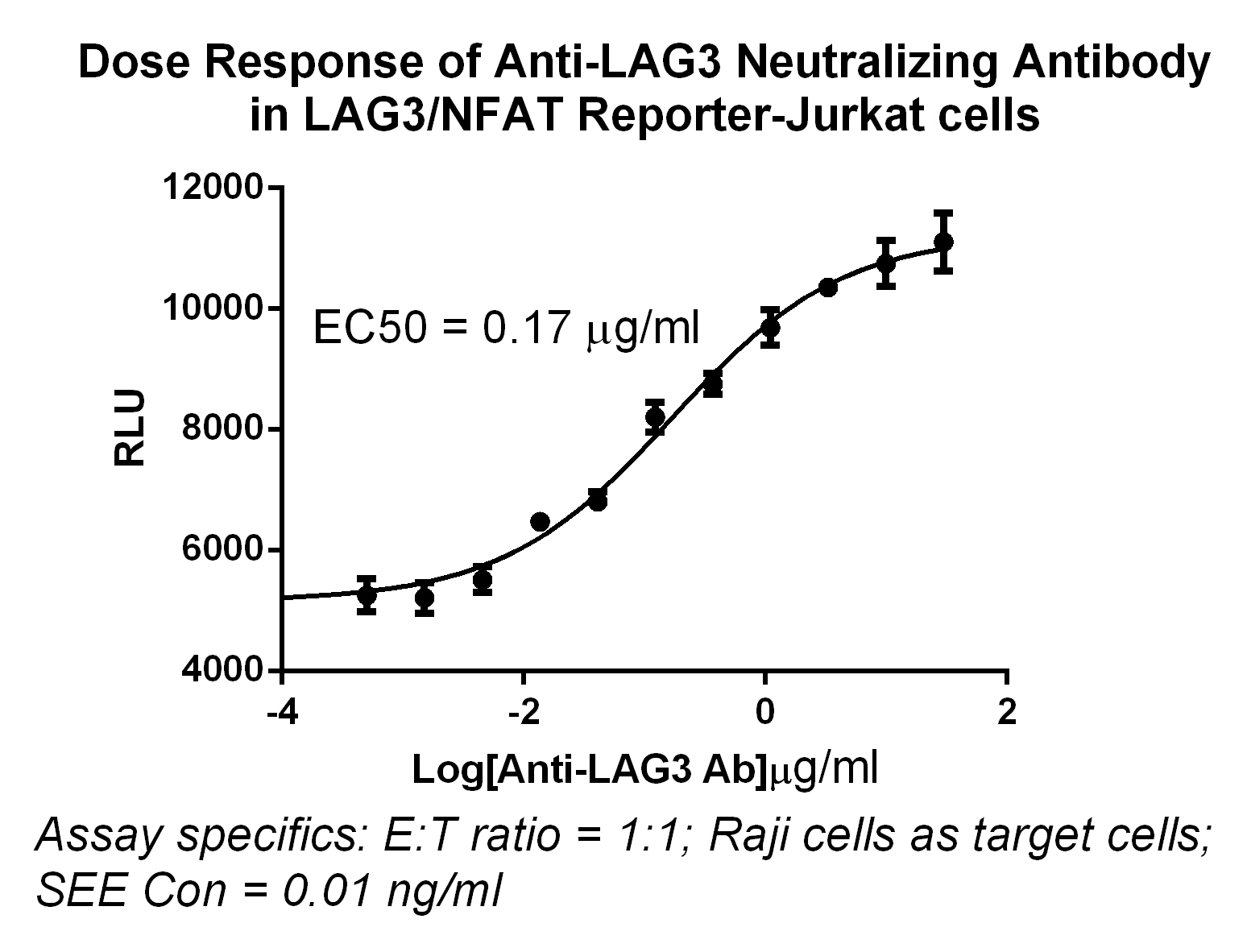
Figure 5. Detect Luciferase assay by Promega Bright-Glo Luciferase Assay System. Jurkat-NFAT-LAG3-Luciferase Reporter cells were stimulated by Jurkat cells,the EC50 was 0.17μg/ml.
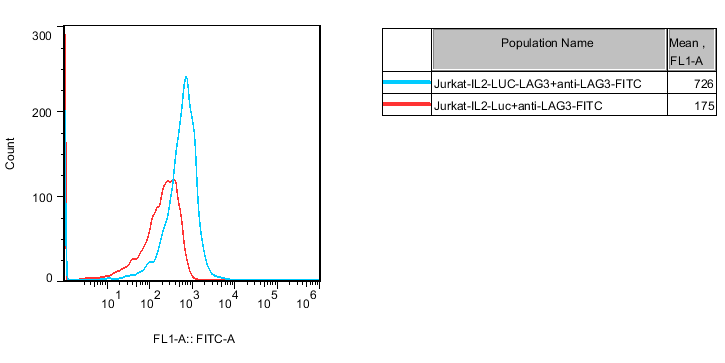
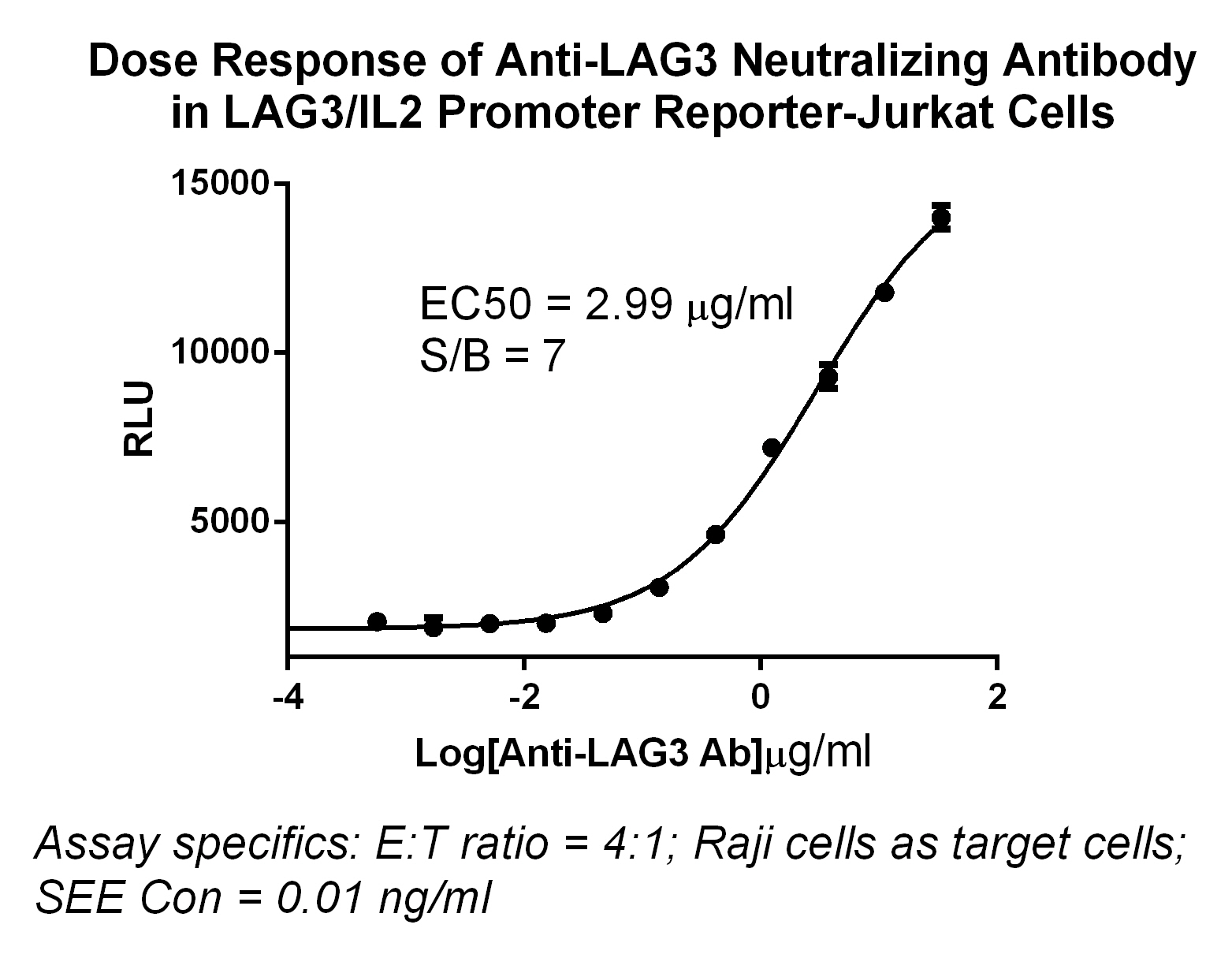
Figure 6. Dose Response of Anti-LAG3 Neutralizing Antibody in LAG3/lL2 Promoter Reporter-Jurkat Cells, the EC50=2.99μg/ml.

